Galeazzi’s test – a useful assessment method for paediatric limb length inequality.
Description
The Galeazzi test, sometimes called Allis sign or Skyline test, is typically used to assess hip dislocation, specifically testing for developmental dysplasia of the hip (DDH), and can also be used to assess significant leg length inequality.
The examination is performed with the child lying supine and their hips flexed to 45 degrees with knees flexed to 90 degrees, and feet on examining table. In this position, look for symmetry in the level of the knees (quickly, in wriggly little children, and repeat two – three times for consistency).
Galeazzi’s test is positive if the height of the knees is asymmetrical (Fig 1), and may be due to: hip dislocation, DDH, congenital femoral shortening, fracture, other congenital conditions (as illustrated in the case example, Figs 1-4).
It is also helpful in determining whether the leg length inequality is primarily from the femur or the tibia, and can be used to assess leg length with knee or hip flexion contracture.
Clinical Notes
- Bilateral hip dislocation may not show a positive Galeazzi sign.
- Galeazzi’s test can be extended to assess adults leg length. The knee shifts proximally (cephalad) with reduced femoral length, and distally (caudally) with a shortened tibia.
- If Galeazzi’s test is positive for limb length inequality, also assess limb girth re atrophy.
Who was Galeazzi?
Professor Riccardo Galeazzi (1866–1952) was one of Italy’s most distinguished orthopaedic surgeons who contributed to clinical and academic medicine in many ways. Galeazzi was one of Italy’s pioneering orthopaedic surgeons, with an extensive bibliography that included nearly 150 publications – truly remarkable for the time, before the ease of electronics and word processing computers.
Professor Galeazzi directed the Orthopaedic clinic at the University of Milan for 35 years. He was known for his work on congenital hip dislocation, scoliosis, skeletal tuberculosis, achondroplasia, osteitis fibrosa cystica and juvenile osteochondritis. Following review of more than 12,000 congenital hip dislocations, he developed the eponymous Galeazzi Test to improve early detection.
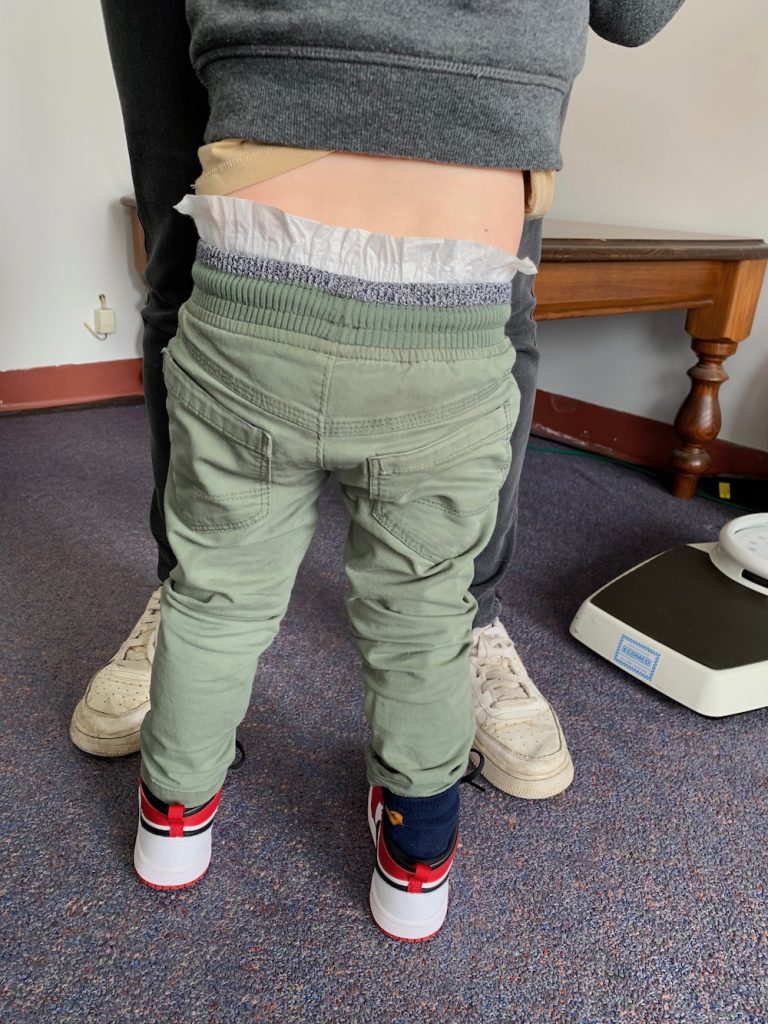
Case example
A 2 year old boy with R congenital hypoplasia, exhibiting four toes R foot, R leg shortened.



- Figure 1 – positive Galeazzi sign (tibial > femoral shortening)
- Figure 2 – R foot hypoplasia
- Figure 3 – stance with in-shoe raise R
- Figure 4 – PSIS level in stance, with R full-length raise
These simple clinical tests are useful when examining paediatric leg length differences. Including post fracture. With all the usual reservations and caveats about a single test needing to be considered in context, rather than being diagnostic, I find that Galeazzi’s test remains helpful, and is very clear to demonstrate to parents to assist explanations and shared decisions.
Whatever the result of Galeazzi’s test clinically, stance and gait are also essential observations, and this entails, gait that is barefoot, shod (various shoes), normal walking pace, and running as relevant.
Check the history – as is always the case, most pertinent information can be found there, and increased suspicion for DDH has traditionally included these factors:
- family history of DDH
- child is first born
- child is female
- breech presentation at birth
- large birth weight (> 4 kgs)
DDH and gender
A recent large retrospective study found DDH to be determined in 149 (3.37%) of 4415 infants, with specific gender differences [Ref 3].
| male | female | |
| Gestational week | ✓ | ✓ |
| Family history | ✓ | |
| Breech presentation | ✓ | ✓ |
| Swaddling/wrap method | ✓ | |
| Congenital knee dislocation | ✓ | |
| Limited hip abduction | ✓ | ✓ |
| Birth weight | ✓ | |
| Multiple pregnancy | ✓ | |
| Oligohydramnios | ✓ | |
| Torticollis | ✓ | |
| CTEV (clubfoot) | ✓ |
References
- Storer, SK. Skaggs, DL. Developmental Dysplasia of the Hip.Am Fam Physician. 2006 Oct 15;74(8):1310-1316. https://www.aafp.org/afp/2006/1015/afp20061015p1310.pdf.
- McCarthy JJ, MacEwen GD, Management of Leg Length Inequality , J South Orthop Assoc. 2001;10(2)
- Onay T et al, J Paediatr Child Health 55:168–174, 2019]
Evidence Essentials is non-profit, with proceeds directed to APERF (Australasian Podiatric Education and Research Foundation) https://www.podiatry.org.au/about/aperf/aperf505
Please keep an eye out for the Evidence Essentials blogs – every month or so – and enjoy the FREE resources https://angelaevanspodiatrists.com.au/category/resources/
Thank you for reading this Evidence Essentials blog post.
Kind regards,
Angela Evans
Dr Angela Evans AM
PhD, FFPM RCPS(Glasg)
www.angelaevanspodiatrists.com.au
